Lymphovenous bypass surgery is a cutting-edge treatment option for early-stage lymphedema. This surgical intervention has revolutionized the management of lymphedema by creating new pathways for lymphatic fluid to flow around blocked areas directly into the venous system. The success of this procedure can significantly enhance the quality of life for patients with lymphedema. Understanding the factors that influence the success of this surgery is crucial for both patients and healthcare providers.
Another important factor in the success of lymphovenous bypass surgery for breast cancer patients is the timing of the procedure. Early intervention for breast cancer-related lymphedema using microlymphaticovenous anastomosis or super microsurgical lymphaticovenular anastomosis has shown promising results in the prevention of breast cancer-related lymphedema. This suggests that lymphatic venous anastomosis may be most effective when performed soon after the onset of limb lymphedema in patients with breast cancer.
Several factors were found to influence the success of the surgery. The number and patency of lymphovenous anastomoses, the technique used (such as lymphaticovenous anastomosis or lymphaticovenular anastomosis), and the experience of the plastic surgery team performing the procedure all played a role in determining the success of the surgical treatment of lymphedema. Additionally, the presence of cancer treatment-related factors, such as lymphedema after breast cancer treatment, could impact the outcomes of the surgery.
What is Lymphovenous Bypass Surgery?
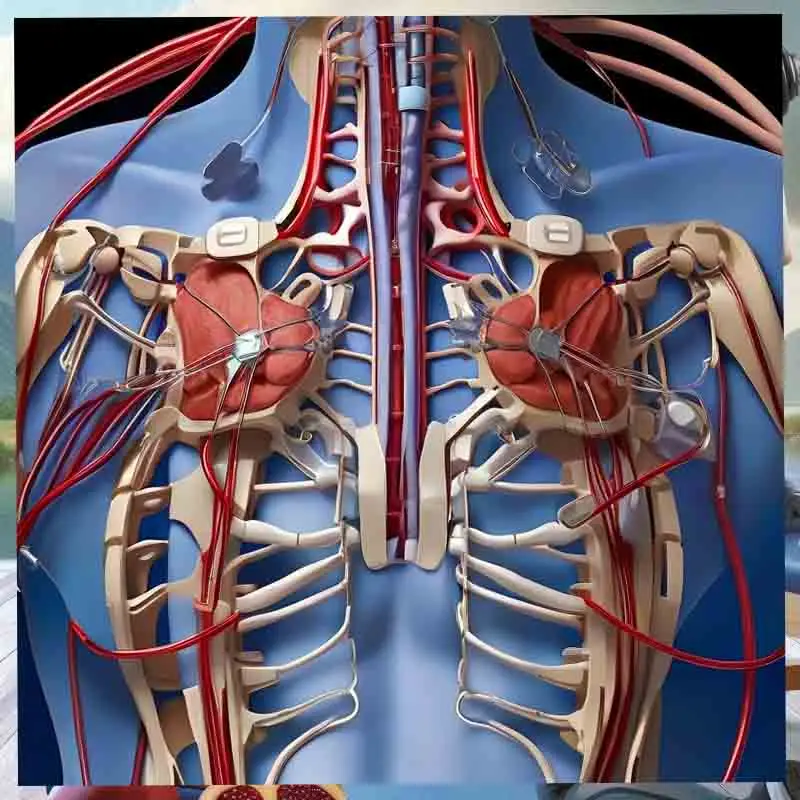
Lymphovenous bypass surgery involves the use of microsurgical techniques to connect lymphatic vessels directly to nearby veins, bypassing damaged or blocked lymphatic pathways. This procedure aims to reduce swelling and improve the flow of lymphatic fluid, offering relief from the chronic symptoms of lymphedema. Early intervention with this surgery is crucial, as it provides the best chance for successful outcomes and can allow patients to become free from the need for compression garments and manual lymphatic drainage (MLD).
Key Factors Influencing Surgical Success
Early Diagnosis and Intervention
Early diagnosis and intervention are paramount for the success of lymphovenous bypass surgery. When lymphedema is identified and treated in its early stages, there is less secondary tissue damage, such as fibrosis, which can complicate surgical outcomes. Early surgical intervention offers the highest probability of long-term relief and improved quality of life.
Surgical Expertise and Technique
The skill and experience of the surgical team are critical factors in determining the success of lymphovenous bypass surgery. Surgeons proficient in supermicrosurgical techniques and with a deep understanding of the lymphatic system’s anatomy can achieve more precise and effective results. The meticulous nature of these surgeries directly impacts the success rate and long-term benefits for the patient. However, one must be aware that many microsurgeons have not gone for specialized super microsurgical or lymphedema surgery training but profess to do lymphovenous bypasses. Do look up the credentials of your healthcare provider.
Patient Selection
It is essential to select the right patients for lymphovenous bypass surgery. Ideal candidates are typically those in the earlier stages of lymphedema, where the lymphatic vessels are still functional and minimal fibrotic tissue exists. Detailed diagnostic assessments, including imaging studies such as lymphoscintigraphy or indocyanine green (ICG) lymphography, are used to evaluate the functionality of lymphatic vessels and determine their suitability for surgery.
Postoperative Care
Effective postoperative care is crucial for the success of lymphovenous bypass surgery. This includes diligent monitoring for complications, regular follow-up appointments, and adherence to compression garment protocols. Post-surgery therapy, such as manual lymphatic drainage (MLD) and personalized exercise programs, can significantly influence long-term outcomes by maintaining the benefits of the surgery and preventing the recurrence of symptoms.
Supporting Techniques to Enhance Outcomes
Integration with Conservative Therapies
Combining lymphovenous bypass surgery with ongoing conservative therapies, such as compression therapy and MLD, enhances the effectiveness of the surgical intervention. This integrated approach helps maintain the surgical gains by continuing to stimulate lymphatic drainage and preventing fluid accumulation.
H3: Technological Advances in Surgical Procedures
Advancements in medical technology, including high-definition microscopes and refined microsurgical tools, have improved the precision and effectiveness of lymphovenous bypass surgeries. These technological enhancements facilitate more accurate vessel connections and reduce surgical risks, contributing to better patient outcomes.
Patient Education and Lifestyle Adjustments
Educating patients about the importance of lifestyle adjustments post-surgery can further improve outcomes. Maintaining a healthy weight, engaging in regular lymphedema-specific exercises, and practicing diligent skin care to prevent infections are crucial. Patients should also be taught self-care practices that help them manage their condition independently.
Challenges and Considerations
Complexity of Lymphatic Disease
Lymphedema can vary significantly in its presentation and progression among patients, adding complexity to its treatment with lymphovenous bypass surgery. Surgeons must tailor their approaches based on individual patient needs and the specific characteristics of their lymphatic damage. A thorough understanding of the disease’s complexity is essential for devising effective treatment strategies.
Long-term Management
While lymphovenous bypass surgery can significantly reduce the symptoms of lymphedema, it is not a cure. Patients must continue with lifelong management of the condition, including the use of compression garments and participation in physical therapy. Long-term management strategies should be designed to maintain the benefits of the surgery and prevent the recurrence of symptoms.
Conclusion
Lymphovenous bypass surgery represents a significant advancement in the treatment of lymphedema, particularly when performed early in the disease process. The success of this procedure depends on multiple factors, including early diagnosis, surgical expertise, comprehensive patient evaluation, and diligent postoperative care. By understanding and optimizing these factors, healthcare providers can offer effective solutions that improve the lives of patients dealing with the chronic challenges of lymphedema. The goal is to provide patients with the best possible outcomes, including the potential to live compression-free, by leveraging the benefits of early surgical intervention and integrated care strategies.
FAQ:
Q: What is lymphovenous bypass surgery?
A: Lymphovenous bypass surgery is a surgical procedure used to treat lymphedema. It connects lymphatic vessels and veins, allowing lymph fluid to drain more effectively.
Q: How does lymphovenous bypass surgery help in the management of lymphedema?
A: Lymphovenous bypass surgery helps manage lymphedema by improving lymphatic drainage, reducing swelling, and improving overall symptoms.
Q: What factors influence the success of lymphovenous bypass surgery?
A: Factors influencing the success of lymphovenous bypass surgery include the number of anastomoses created, the severity and duration of lymphedema, and the surgical team’s expertise performing the procedure.
Q: Is lymphovenous bypass surgery effective for breast cancer treatment-related lymphedema?
A: Lymphovenous bypass surgery has shown effectiveness in treating breast cancer treatment-related lymphedema by improving lymphatic drainage and reducing swelling in the affected limb.
Q: What is the role of lymphaticovenular anastomosis in the treatment of lymphedema?
A: Lymphaticovenular anastomosis is a technique used in lymphedema management. In this technique, lymphatic vessels are connected directly to veins to improve lymphatic flow and reduce swelling.
Q: How are the outcomes of lymphovenous anastomosis measured?
A: The outcomes of lymphovenous anastomosis are typically measured based on improvements in limb circumference, reduction in lymphedema severity, and overall enhancement in the quality of life for lymphedema patients.
Q: What is the difference between lymphaticovenular bypass and lymphaticovenous anastomosis?
A: Lymphaticovenular bypass and lymphatic venous anastomosis are similar procedures that involve connecting lymphatic vessels to veins. However, they may differ in the specific techniques used and the placement of the anastomoses.