Understanding Lymphedema and the Lymphatic System: A Deep Dive
When discussing health and wellness, the lymphatic system doesn’t always get the attention it deserves. However, this vital part of the body’s immune system plays a significant role in keeping us healthy. If you’ve ever experienced or heard about lymphedema, you know how this condition can impact daily life. Let’s deeply dive into lymphedema and its connection to the lymphatic system, exploring its causes, symptoms, treatments, and ways to manage it.
Key Takeaways
- Lymphedema is a chronic condition characterized by swelling due to issues with the lymphatic system.
- Cancer treatment, infections, or congenital factors can cause it.
- Management includes compression garments, skin care, and therapies like manual lymphatic drainage.
- Early diagnosis and treatment can improve the quality of life for people with lymphedema.
What is Lymphedema and How Does It Affect the Lymphatic System?
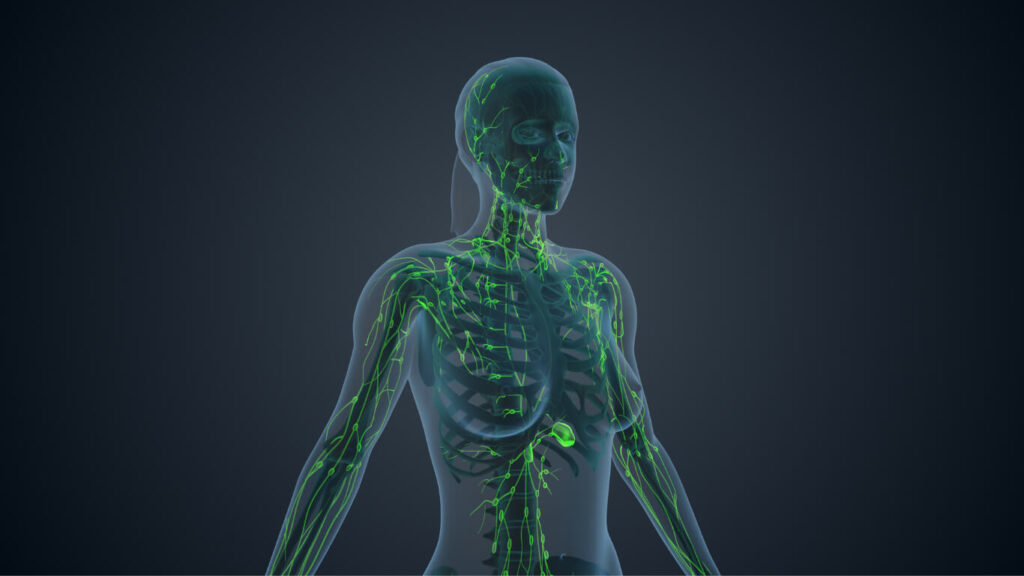
Lymphedema happens when the lymphatic system doesn’t function properly. This condition leads to the accumulation of lymph fluid in parts of the body, most commonly an arm or leg, causing swelling and other symptoms. Lymphedema is swelling that often results from damage to the lymphatic system or blockages in the lymphatic vessel network.
The lymphatic system works hand-in-hand with the circulation system to move fluid throughout the body and filter harmful substances. When this system is compromised, lymphatic fluid builds up, leading to swelling and potentially permanent damage to surrounding tissue. This condition can also affect other areas of the body and may develop over time, especially years after treatment for cancer or other conditions.
What Are the Symptoms and Causes of Lymphedema?
Symptoms of Lymphedema
The signs of lymphedema can vary depending on its severity, but common symptoms may include:
- Persistent swelling in an arm or leg.
- A heavy or tight feeling in the affected limb.
- Tissue that may feel firmer or hardened.
- Recurring infections.
- Reduced mobility in the affected area.
These symptoms and causes are often subtle initially, so it’s crucial to talk to your doctor if you notice any unusual changes in your body.
Causes of Lymphedema
The causes of swelling due to lymphedema include two primary types:
- Primary lymphedema: This rare condition is inherited and caused by issues in the lymphatic system development.
- Secondary lymphedema: This more common form arises from damage to the lymphatic system, such as after cancer treatment, surgery, or infections.
Understanding these causes helps identify potential risks and address the condition early.
How Does Lymphedema Develop in the Body?
Lymphedema occurs when the lymphatic system is damaged or overwhelmed. The condition often starts with minor swelling that can progress if untreated. Here’s a closer look:
- Early Stages: Fluid begins to collect in specific body areas, leading to mild swelling that may come and go.
- Progression: Over time, the lymph fluid throughout the body becomes harder to manage, causing the affected area to swell consistently.
- Advanced Stages: In severe cases, the skin and underlying tissue can thicken, and the area may become prone to infections.
Knowing the stages of lymphedema is essential for effective management and intervention.
What Types of Lymphedema Exist?
Primary Lymphedema
This type is rare and results from genetic issues that affect the development of the lymphatic system. It may present at birth or later in life.
Secondary Lymphedema
This form is much more common and is often triggered by cancer surgery, radiation therapy, or infections that damage lymph nodes and lymphatic vessels. Conditions such as breast cancer and skin cancer significantly increase the risk of developing lymphedema.
What Are the Common Risk Factors for Lymphedema?
What is the Risk of Developing Lymphedema After Cancer Treatment?
One of the leading causes of secondary lymphedema is cancer and cancer treatment. Surgeries involving lymph node transfer or removal, radiation, and chemotherapy can disrupt the lymphatic system, increasing the risk of lymphedema. This risk is particularly high for individuals undergoing treatment for breast cancer or melanoma.
How Does Damage to the Lymphatic System Contribute to Lymphedema?
The lymphatic system is part of a complex network of vessels and nodes responsible for moving lymph fluid throughout the body. When this network is damaged, it disrupts the drainage process, causing fluid to accumulate. Trauma, infection, or surgical procedures can cause damage to the lymphatic system.
What Roles Do Lymph Nodes and Lymphatic Vessels Play?
Lymph nodes filter harmful substances, while lymphatic vessels transport the lymph fluid. Together, they maintain fluid balance and support the body’s immune system. When either is compromised, lymphedema can occur in the affected area.
How Is Lymphedema Diagnosed?
What Are the Steps in a Lymphedema Diagnosis?
Diagnosing lymphedema involves a combination of medical history, physical exams, and diagnostic imaging. A doctor will:
- Review your symptoms and potential risk factors.
- Conduct a physical exam to assess the signs of lymphedema, including swelling and tissue changes.
- Order imaging tests for a clearer picture of the affected area.
What Tests Are Used to Assess Lymphedema?
Common diagnostic tools include:
- Lymphoscintigraphy: This imaging test maps the flow of lymph fluid.
- MRI or CT scans: Detailed images of areas inside the body to detect blockages or damage.
- Ultrasound: Identifies fluid buildup and examines surrounding tissue.
These tests help confirm a lymphedema diagnosis and guide appropriate treatment.
What Are the Treatment Options for Lymphedema?
What is the Role of a Certified Lymphedema Therapist?
A certified lymphedema therapist specializes in managing the condition through techniques like manual lymphatic drainage and designing personalized care plans. Working with a specialist can improve outcomes and quality of life.
How Can Compression Garments Help Manage Lymphedema?
Compression garments apply gentle pressure to the affected area, reducing swelling and encouraging proper fluid movement. These garments are an essential tool for managing lymphedema symptoms.
What Are the Surgical Treatment Options for Lymphedema?
For severe cases, surgical treatment of lymphedema includes procedures like:
- Lymphatic bypass: Reconnecting lymphatic vessels to improve drainage.
- Vascularized lymph node transfer: Transferring healthy lymph nodes to the affected area.
How Can One Manage Lymphedema daily?
What Lifestyle Changes Can Help Reduce Swelling?
Lifestyle adjustments, such as maintaining a healthy weight, exercising regularly, and avoiding tight clothing, can reduce swelling and improve overall health.
How Important is Skin Care in Managing Lymphedema?
Proper skin care prevents infections and keeps the tissue healthy. Moisturizing daily and protecting against cuts or scrapes are simple yet effective measures.
What Techniques Can Be Used for Manual Lymphatic Drainage?
Manual lymphatic drainage is a gentle massage technique a certified lymphedema therapist performs to encourage fluid movement and alleviate swelling.
What Are the Long-Term Implications of Living with Lymphedema?
How Does Lymphedema Affect Quality of Life?
Living with lymphedema can affect mobility, self-esteem, and mental health. The condition’s physical and emotional toll underscores the importance of comprehensive care.
What Are the Psychological Effects of a Lymphedema Diagnosis?
Being diagnosed with lymphedema can be overwhelming, leading to anxiety or depression. Support groups and counseling can help individuals cope.
What Support Systems Are Available for Those with Lymphedema?
Resources like support groups, online forums, and organizations provide valuable assistance and community for people with lymphedema.
FAQs
Can Lymphedema Be Prevented?
Taking proactive measures, such as skin care and regular exercise, can greatly decrease the risk of lymphedema.
What Is the Difference Between Primary and Secondary Lymphedema?
Primary lymphedema is genetic, while external factors like cancer surgery or infections cause secondary lymphedema.
How Painful Is Lymphedema?
Lymphedema can be painful, especially in advanced stages, but proper management can alleviate discomfort.
How Long Does It Take for Lymphedema to Develop?
Some people may develop lymphedema shortly after an injury or surgery, while others may experience it years after treatment.