Lymphedema vs. Edema: Unmasking the Hidden Differences in Chronic Swelling
Swelling in the body can be confusing, especially when differentiating between lymphedema vs edema. Both conditions involve fluid retention, but their causes, symptoms, and treatments are distinct. Whether you’ve experienced swelling firsthand or want to understand these conditions better, this article will help you learn the critical differences between lymphedema and edema.
Key Takeaways
- Lymphedema is often associated with damage to the lymphatic system, while edema results from fluid retention due to other underlying conditions.
- Identifying symptoms of lymphedema early and seeking a proper diagnosis can prevent complications.
- Edema is caused by heart disease, kidney problems, or venous insufficiency, while secondary lymphedema often arises after cancer treatment.
- Treatment options include compression therapy, lifestyle changes, and in some cases, manual lymphatic drainage.
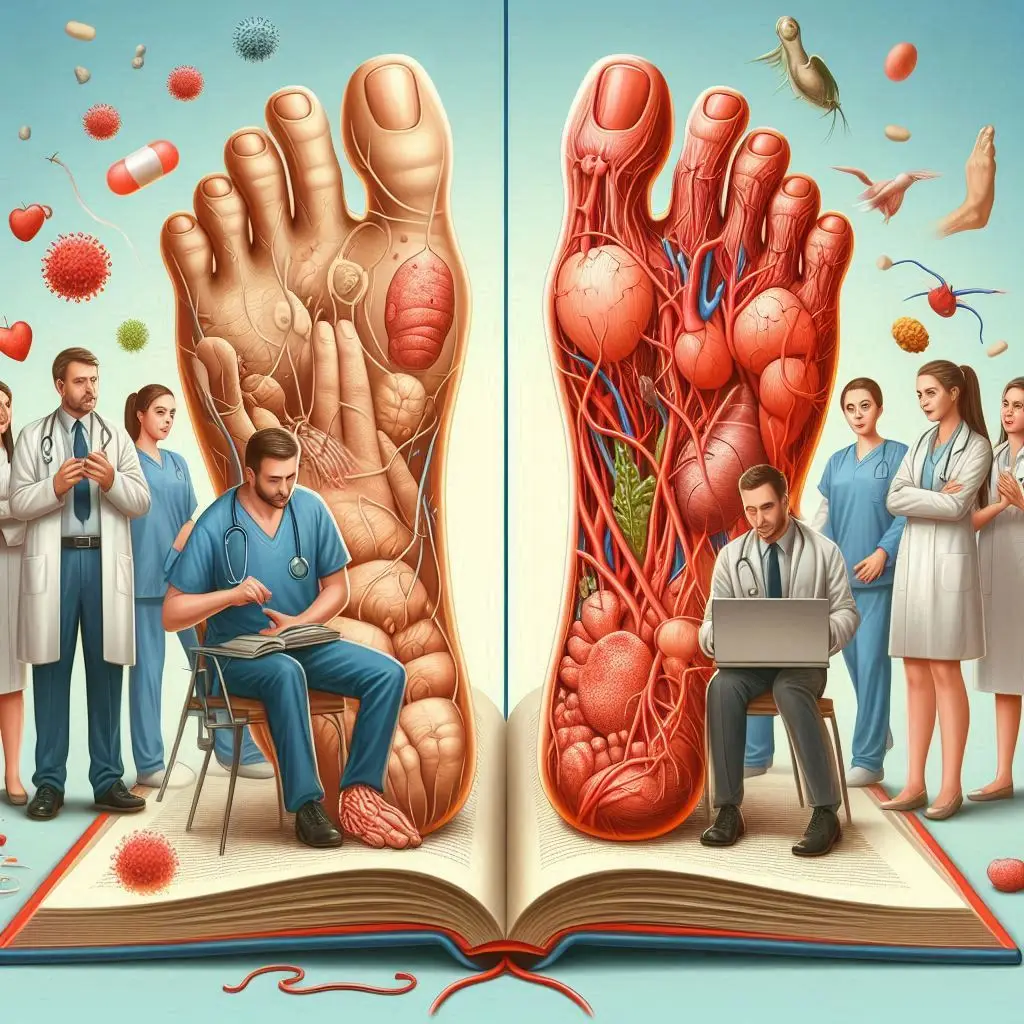
What Are the Key Differences Between Lymphedema and Edema?
Understanding the underlying causes of lymphedema and edema
The difference between edema and lymphedema starts with their causes. Lymphedema is caused by damage to the lymphatic system, leading to lymphatic fluid accumulation in the tissues. Secondary lymphedema often develops after surgeries like breast cancer-related lymphedema or treatments involving lymph node removal or radiation.
In contrast, edema occurs when excess fluid accumulates in the tissues due to heart failure, kidney disease, or chronic venous insufficiency. Both situations involve swelling, but they require different approaches to diagnosis and treatment.
Distinguishing symptoms: How to tell lymphedema from edema
One way to distinguish lymphedema vs edema is by how the swelling behaves. Pitting edema occurs when pressure on the swollen area leaves a dent or pit, indicating fluid accumulation. On the other hand, lymphedema is often non-pitting, and the swelling leaves a mark only in advanced stages.
Patients with lymphedema may notice heaviness, thickened skin, or lymphedema symptoms like infections. Edema usually affects both sides of the body, legs and feet, whereas lymphedema can occur unilaterally in arms or legs.
The role of the lymphatic system in lymphedema vs. edema
The lymphatic system plays a crucial role in lymphedema management. In cases of lymphedema, damaged lymphatic vessels prevent the normal flow of lymph, leading to chronic lymphedema. Meanwhile, edema fluid results from an imbalance in the circulatory or kidney systems.
While lymphedema is a chronic condition directly linked to the lymphatic system, edema typically resolves if the underlying cause, such as heart failure or kidney issues, is treated.
How Are Lymphedema and Edema Diagnosed?
Diagnostic techniques for identifying lymphedema
The diagnosis of lymphedema involves a certified lymphedema therapist, who may assess limb circumference and check for skin thickening. Advanced lymphedema might require imaging tests like lymphoscintigraphy to identify blockages in the lymphatic channels.
Evaluating edema: Pitting vs. non-pitting edema
Doctors differentiate between pitting edema and non-pitting edema by applying pressure to the affected area. Pitting edema is more common in conditions like heart failure, while lymphedema progresses without leaving a pit in early stages. This difference helps doctors diagnose lymphedema accurately.
When to consult a certified lymphedema therapist
If body swelling persists after injury or cancer treatment, it’s essential to consult a lymphedema specialist. A certified lymphedema therapist can create a personalized care plan that includes decongestive therapy and manual lymphatic drainage.
What Are the Stages of Lymphedema and How Do They Differ from Edema Progression?
Understanding the four stages of lymphedema
The stages of lymphedema range from mild to severe:
- Stage 0: Latent stage with no visible swelling.
- Stage 1: Mild swelling that can reduce with rest or elevation.
- Stage 2: Persistent swelling with tissue thickening and excess fluid.
- Stage 3: Severe chronic lymphedema (elephantiasis), marked by hardened skin and deformity.
Comparing lymphedema stages to edema severity
While lymphedema stages follow a progressive pattern, edema usually resolves if treated promptly. Edema and lymphedema differ in progression; edema can also worsen temporarily but does not result in permanent skin changes like lymphedema may.
What Treatment Options Are Available for Lymphedema and Edema?
Compression therapy: Benefits for both lymphedema and edema
Compression therapy is effective in managing both lymphedema and edema. It helps reduce swelling by improving fluid movement through vessels and veins. Patients often wear compression garments to reduce swelling and prevent fluid buildup.
Manual lymphatic drainage techniques
Manual lymphatic drainage promotes the movement of lymphatic fluid through the body’s natural pathways. This therapy is often included in decongestive therapy for lymphedema management.
Medication and lifestyle changes for managing edema
In cases of edema, doctors may prescribe diuretics to remove excess fluid and suggest lifestyle changes, such as reducing salt intake and elevating the legs and feet. Due to venous insufficiency, patients with chronic edema should also wear compression stockings to reduce fluid retention.
Can Lymphedema Be Prevented, and How Does This Differ from Edema Prevention?
Risk factors and prevention strategies for secondary lymphedema
Secondary lymphedema can develop after surgeries involving the removal of lymph nodes, especially in breast cancer-related lymphedema. Prevention strategies include monitoring for early signs, wearing compression garments, and following up with a lymphedema therapist.
Lifestyle modifications to reduce edema risk
To reduce the risk of edema, patients can adopt healthy habits such as regular exercise, maintaining a balanced diet, and avoiding prolonged sitting or standing. Edema may develop due to venous insufficiency, so managing underlying conditions is essential.
How Do Chronic Venous Insufficiency and Lipedema Relate to Lymphedema and Edema?
Distinguishing chronic venous insufficiency from lymphedema
Chronic venous insufficiency causes blood to pool in the veins, leading to swelling. This condition differs from lymphedema, where fluid buildup occurs due to a damaged lymphatic system.
Understanding the connection between lipedema, lymphedema, and edema
Lipedema is a chronic condition characterized by fat buildup, which can resemble lymphedema. However, lipedema and lymphedema can coexist, and both conditions may involve swelling in the legs due to impaired circulation.
What Are the Long-Term Implications of Living with Lymphedema vs. Edema?
Managing chronic lymphedema: Challenges and coping strategies
Patients with chronic lymphedema often face challenges such as recurring infections and limited mobility. Lymphedema management includes compression therapy, manual lymphatic drainage, and regular monitoring by a lymphedema specialist.
Potential complications of untreated edema
If left untreated, edema can lead to severe complications, including ulcers and infections. Edema due to kidney or heart failure requires prompt medical attention to prevent further complications.
Quality of life considerations for lymphedema and edema patients
Patients with lymphedema and chronic edema may experience reduced quality of life. Staying active, following prescribed therapies, and working with healthcare providers can help patients maintain their well-being.
Closing Thought
Understanding the difference between lymphedema vs edema is crucial for effective management. Both conditions involve swelling in the body, but their causes, symptoms, and treatments differ. Whether dealing with edema fluid from an underlying health condition or managing lymphedema after cancer treatment, early detection and the suitable treatment options can make a significant difference. Working closely with a healthcare provider, such as a certified lymphedema therapist, ensures that the appropriate therapies improve patient outcomes and quality of life.
Frequently Asked Questions About Lymphedema vs. Edema
1. What is the critical difference between lymphedema and edema?
The primary difference between lymphedema vs edema lies in their causes. Lymphedema is caused by damage to the lymphatic system, resulting in the buildup of lymphatic fluid in tissues. Edema is swelling caused by an underlying condition such as heart failure, kidney disease, or chronic venous insufficiency, leading to fluid that causes localized or general swelling.
2. How can I tell if my swelling is lymphedema or edema?
In pitting edema, applying pressure to the swelling leaves a mark or pit, which is familiar with heart or kidney conditions. Lymphedema usually presents as non-pitting swelling that feels firm, especially in later stages. It may also involve skin thickening, infections, and heaviness in arms or legs.
3. Can lymphedema occur after cancer treatment?
Yes, cancer-related lymphedema is a common form of secondary lymphedema. It often occurs after the removal of lymph nodes or radiation therapy, especially in breast cancer patients. If left untreated, lymphedema may progress and require lifelong treatment options.
4. What are the treatment options for lymphedema vs. edema?
Both conditions benefit from compression therapy to reduce swelling, but lymphedema treatment may also include manual lymphatic drainage and decongestive therapy. In contrast, edema would often be managed with medications like diuretics, along with lifestyle changes to address underlying causes, such as venous insufficiency.
5. Can lifestyle changes prevent lymphedema and edema?
While primary lymphedema is congenital and not preventable, secondary lymphedema prevention focuses on avoiding infections, wearing compression garments, and monitoring for early signs after cancer treatment. To prevent edema, patients should manage underlying health conditions, stay active, elevate legs and feet, and follow a low-sodium diet to reduce fluid retention.





2 thoughts on “Lymphedema vs. Edema: Key Differences and Care Strategies Explained”
Thank you for all the information. I’ve seen a few doctors and they’ve referred that edema was the problem in both legs. Recently, my Primary Dr said it was not edema but lymphedema. From what I’ve read, that’s more like the symptoms I have. My Dr is making a referral to see a lymphedema specialist and hopefully confirm the diagnosis.
Yes it’s so important to get the right diagnosis! A simple ICG lymphography helps. If that’s not available either lymphoscintigraphy (nuclear scan and less sensitive) or magnetic resonance lymphangiography is ok too