What Causes Lymphedema to Worsen?
Definition of Lymphedema
Lymphedema is a condition that involves the abnormal accumulation of lymphatic fluid in the body’s tissues, resulting in swelling—most commonly in the arms or legs. The lymphatic system maintains the body’s fluid balance by draining excess fluid from tissues and returning it to the bloodstream. When this system is disrupted, fluid accumulates in the affected area, leading to swelling and a range of other symptoms. Lymphedema can develop as a primary condition, often due to genetic factors, or secondary to an underlying cause, such as cancer treatment or surgery.
The condition can manifest in varying degrees, from mild swelling to more severe stages, where the swelling becomes persistent and accompanied by other complications. While lymphedema itself is not life-threatening, it can significantly impact a person’s quality of life, causing discomfort, restricted mobility, and, in some cases, mental health challenges.
Importance of Understanding the Factors That Contribute to Its Worsening
Lymphedema is a chronic condition that requires ongoing management to prevent symptoms from worsening. Understanding the factors contributing to its progression is crucial for patients and healthcare providers. Factors like delayed treatment, lifestyle choices, and medical interventions can all affect the severity of lymphedema symptoms. By recognizing what causes lymphedema to worsen, individuals can make informed decisions about treatment and lifestyle adjustments to manage their condition better and prevent further complications.
Overview of the Blog Post Structure
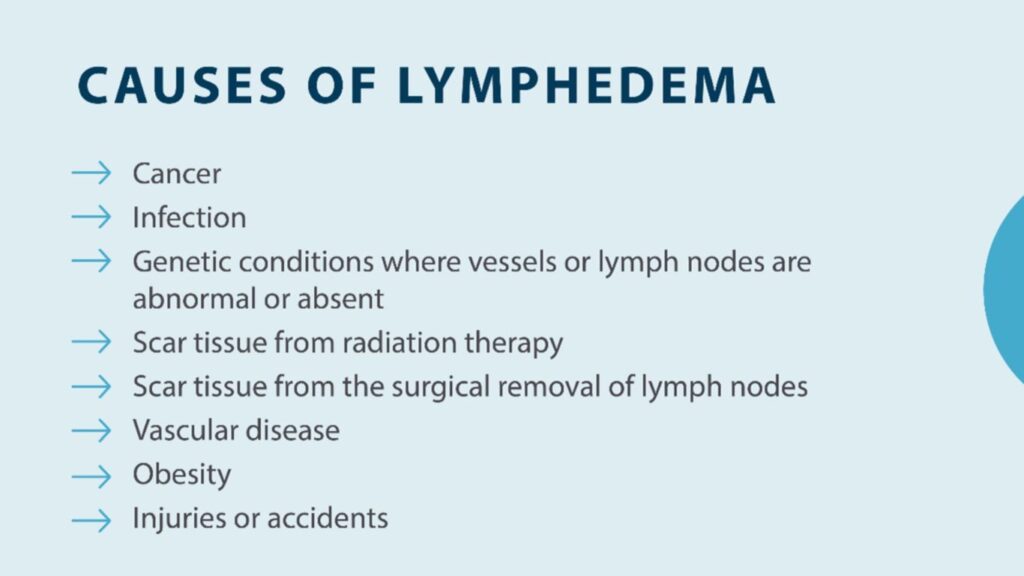
This blog post will explore the primary causes of lymphedema and the factors contributing to its worsening. We will discuss how genetic predispositions, surgical interventions, and radiation therapy contribute to the condition’s development. Additionally, we will examine how lifestyle factors such as obesity, a sedentary lifestyle, and poor skin care can exacerbate symptoms. Environmental and health-related triggers, including infections and weather changes, will also be covered. Finally, we’ll provide actionable advice on managing and preventing worsening symptoms.
Primary Causes of Lymphedema
Genetic Predisposition and Congenital Conditions
Lymphedema can be caused by genetic predispositions, leading to congenital or primary lymphedema. Primary lymphedema occurs when there is a malformation in the lymphatic system from birth, resulting in inadequate lymphatic vessels or impaired lymphatic flow. This type of lymphedema is relatively rare but can develop at any age, with some individuals noticing symptoms in childhood (lymphedema praecox) and others in adulthood (lymphedema tarda).
The lymphatic system, which consists of vessels and lymph nodes that help remove waste and fluid from tissues, may be underdeveloped in individuals with primary lymphedema. When the system fails to drain excess fluid adequately, it accumulates in the affected area, causing swelling and an increased risk of infection. Genetic conditions such as these can cause lymphedema, making individuals more susceptible to fluid buildup from an early age.
Surgical Interventions and Their Impact on Lymphatic Function
Surgical interventions are one of the most common causes of secondary lymphedema. Procedures that involve the removal of lymph nodes—such as those performed during cancer treatments—can compromise lymphatic drainage and lead to the development of lymphedema. For example, breast cancer treatment often requires the removal of lymph nodes under the arm, which impairs the flow of lymphatic fluid from the arm or chest area, leading to swelling in the affected area.
In some cases, lymphedema can occur immediately following surgery, but it may also develop months or even years later, mainly if there are complications related to the healing process. Surgical scars can also restrict the flow of lymph, further exacerbating symptoms. As a result, patients who undergo cancer treatments or other surgeries involving lymph node removal should be monitored for signs of lymphedema and receive appropriate care to prevent worsening symptoms.
Radiation Therapy and Its Effects on Lymphatic Tissues
Radiation therapy, often used in cancer treatment, is another significant factor in the development and worsening of lymphedema. Radiation can damage lymphatic vessels and nodes, impairing the system’s ability to drain lymph fluid properly. As a result, radiation therapy increases the risk of lymphedema in areas where the lymphatic system has been damaged. This is particularly common in patients who have received radiation treatment for breast cancer, head and neck cancers, or pelvic cancers.
Radiation-induced damage to lymphatic tissues can lead to lymph stasis, where lymph fluid accumulates in the tissues. In addition to the direct effects of radiation on the lymphatic system, the resulting scarring can further hinder lymphatic drainage and cause the condition to worsen over time. For patients undergoing radiation, managing and monitoring the lymphatic system to prevent or mitigate lymphedema is critical.
Lifestyle Factors Contributing to Lymphedema to Worsen
Obesity and Its Role in Lymphatic Drainage
Obesity is a significant risk factor for worsening lymphedema. Excess body fat can put additional pressure on the lymphatic system, making it more difficult for lymph fluid to be adequately drained from tissues. When the lymphatic vessels are under stress from excess weight, they may become less efficient at moving fluid, leading to increased swelling in the affected areas.
Additionally, the excess fat can obstruct lymphatic vessels, exacerbating the symptoms of lymphedema. Managing weight through diet and exercise is essential to preventing lymphedema’s progression. Maintaining a healthy weight helps reduce the strain on the lymphatic system, allowing it to function more effectively and preventing further fluid buildup.
Sedentary Lifestyle and Reduced Physical Activity
A sedentary lifestyle can contribute to the worsening of lymphedema by impairing lymphatic circulation. The lymphatic system relies on muscle contractions and movement to propel lymph fluid. When a person is inactive for extended periods, the flow of lymph fluid is reduced, leading to fluid accumulation in the affected areas.
Regular physical activity promotes healthy lymphatic drainage, including walking, swimming, and low-impact exercises. Exercise helps move lymph fluid, reduce swelling, and improve overall circulation. For individuals with lymphedema, engaging in activities encouraging movement and flexibility can significantly alleviate symptoms and prevent the condition from worsening.
Poor Skin Care and Hygiene Practices
Poor skincare and hygiene practices can also contribute to the worsening of lymphedema. The skin in the affected area is often more vulnerable to infection, irritation, and injury, and maintaining proper skin care is essential to prevent complications. If an individual with lymphedema develops cuts, scratches, or infections, these can lead to further swelling and inflammation, exacerbating the condition.
Proper hygiene, including daily washing with soap and water, moisturizing the skin, and avoiding harsh chemicals or fragrances, is key to preventing skin infections. It is also essential for individuals with lymphedema to avoid prolonged sun exposure or extreme temperatures, as these can irritate the skin and worsen swelling.
Environmental and Health-Related Triggers
Infections and Their Impact on Lymphatic Health
Infections are one of the most common triggers for worsening lymphedema. An infection in an area affected by lymphedema can cause inflammation and fluid retention, leading to increased swelling. Cellulitis, a bacterial skin infection, is particularly common in individuals with lymphedema and can cause significant complications. The lymphatic system plays a role in fighting infections, but when compromised, it can effectively manage the body’s immune response.
Individuals with lymphedema must seek medical attention immediately if they notice signs of infection, such as redness, heat, or pain in the affected area. Early antibiotic intervention can help prevent infections from worsening and reduce the risk of further lymphatic damage.
Inflammatory Conditions and Their Exacerbation of Symptoms
Chronic inflammatory conditions, such as rheumatoid arthritis or other autoimmune disorders, can exacerbate the symptoms of lymphedema. Inflammation can worsen the compromised lymphatic drainage, increasing swelling and fluid retention in the affected areas. Additionally, inflammation can contribute to the progression of fibrosis, a condition where the tissue becomes thickened and scarred, further hindering lymphatic flow.
Managing chronic inflammation through medication, physical therapy, and lifestyle changes can help reduce its impact on lymphedema. Individuals with lymphedema and inflammatory conditions should work closely with their healthcare providers to develop a comprehensive treatment plan.
Weather Changes and Their Influence on Swelling
Weather changes, particularly heat and humidity, can also trigger worsening symptoms of lymphedema. Hot weather can cause blood vessels to expand, leading to increased swelling, while moisture can make it more difficult for the body to regulate fluid balance. Cold weather, on the other hand, can cause the lymphatic vessels to constrict, slowing lymphatic drainage.
Individuals with lymphedema should take extra precautions during extreme weather conditions. Wearing compression garments, staying hydrated, and avoiding prolonged exposure to heat or cold can help prevent swelling from worsening during these times.
Conclusion
Recap of the Key Factors That Can Worsen Lymphedema
Lymphedema can worsen due to a combination of medical interventions, lifestyle choices, and environmental factors. Surgical procedures, radiation therapy, obesity, lack of physical activity, poor skin care, and infections are all significant contributors to the progression of lymphedema. Understanding these factors is key to preventing worsening symptoms and managing the condition effectively.
FAQs
Q: What is lymphedema and how does it develop?
A: Lymphedema is a condition characterized by the build-up of fluid throughout the body, typically affecting the arms and legs. It can develop when the lymphatic system is damaged or blocked, preventing the normal drainage of lymph fluid.
Q: What are the common symptoms and causes of lymphedema?
A: Symptoms of lymphedema include swelling, discomfort, and a feeling of heaviness in the affected area. The causes of swelling can vary, but common triggers include surgery, radiation therapy, or infections that affect the lymphatic system.
Q: How can I manage lymphedema effectively?
A: To manage lymphedema, it’s important to follow a comprehensive treatment plan that may include physical therapy, compression garments, and lifestyle changes. Consulting with a certified lymphedema therapist can provide personalized strategies to ease its symptoms.
Q: What steps can I take to prevent lymphedema from getting worse?
A: Steps to prevent lymphedema from worsening include maintaining a healthy weight, exercising regularly, avoiding injury to the affected area, and following your doctor’s recommendations for monitoring your condition.
Q: When should I talk to my doctor about my lymphedema symptoms?
A: You should talk to your doctor if you notice any changes in your swelling, such as increased fluid throughout the body, changes in skin texture, or new symptoms. Early diagnosis and treatment of lymphedema are crucial for effective management.
Q: What treatments are available for lymphedema?
A: Treatment for lymphedema may include manual lymphatic drainage, compression therapy, exercise, and in some cases, lymphedema surgery, such as lymph node transfer or lymphatic bypass, to improve drainage.
Q: What is lymphedema surgery and when might it be necessary?
A: Lymphedema surgery may be necessary for individuals who do not respond to conservative treatments and experience significant swelling that affects their quality of life. Surgical options aim to reduce swelling and improve lymphatic function.
Q: Can lymphedema affect areas other than the arms and legs?
A: Yes, lymphedema is most common in the arms and legs, but it can also affect other areas of the body, including the abdomen and genitals, depending on the underlying cause and the lymphatic system’s involvement.
Q: How can I find a certified lymphedema therapist?
A: You can find a certified lymphedema therapist by searching through professional organizations that list accredited therapists, such as the Lymphology Association of North America (LANA) or by asking your doctor for recommendations.