Primary Prevention
The prospect of preventing lymphedema is appealing both for surgeons and patients. For patients, it means potentially avoiding the necessity of wearing compression garments for life, while surgeons might be able to limit the extent of invasive and comprehensive surgeries. Primary prevention focuses on avoiding the disease entirely by performing interventions before it occurs.
Identifying risk factors
The key to primary prevention is a robust risk prediction model. However, most models that exist have significant drawbacks and lack accuracy. Hence, no particular model has been recommended.
Having said that, we do know that these risk factors are significant predictors of lymphedema formation:
- An elevated body mass index of more than 25 kg/m2
- Removal of the armpit lymph nodes (axillary dissection) especially if the number is more than 30 nodes
- Radiation therapy
- Chemotherapy before breast cancer removal for more than 144 days ( neoadjuvant chemotherapy)
- Lymph nodes removed from the armpit are positive for cancer
- Postoperative complications like infection, fluid accumulation (seroma), early swelling (edema)
Immediate lymphatic reconstruction
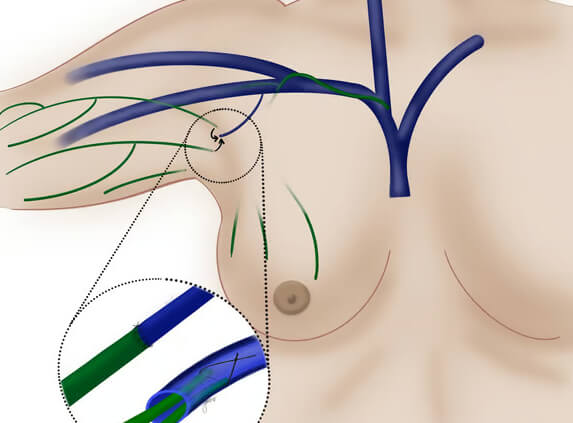
Immediate lymphatic reconstruction involves restoring lymphatic flow after removal of the lymph nodes in the armpit. This can be achieved by lymphovenous anastomosis (LVA) or, more commonly lymphovenous implantation (LVI). This technique was first popularised by Drs. Boccardo and Campisi, and the LVI technique was used to perform the reconstruction. This was termed lymphatic microsurgical preventive healing approach or LYMPHA.
This procedure is generally low-risk and well-tolerated. It is performed at the same time as breast cancer removal. Although most studies have reported good outcomes with immediate lymphatic reconstruction, demonstrating lower probability of lymphedema formation, most of these studies are of low quality with significant risk of bias, short follow-up periods, and inconsistent diagnostic methods.
How is immediate lymphatic reconstruction done?
Severed lymphatics that drain the arm is connected to a nearby vein branch of similar diameter. Typically 1-3 connections are made with the aid of a microscope.
Supermicrosurgical LVA or Telescoped LVI can be used to achieve bypass. Theoretically, LVAs should confer better patency and de-swelling effects of the arm.
In a nutshell
Based on initial research, immediate lymphatic reconstruction seems promising in preventing lymphedema related to cancer treatments. However, we need more high-quality studies to firmly establish this approach as a standard preventative measure. Currently, the research has some limitations, including varied results and short observation periods after the procedure.
Despite these challenges, ILR can still be a valuable option in clinical settings. Doctors can consider this method for patients who are at a higher risk of developing lymphedema. Currently, the absence of a reliable risk prediction model means that there is a potential for conducting unnecessary surgeries, as it is challenging to pinpoint those who are at a high risk of developing lymphedema with precision. In situations where determining a patient’s risk level accurately is not feasible, it is prudent for doctors to consider implementing regular screenings for lymphedema indicators, thereby facilitating early interventions to mitigate its impact on patients. This is why secondary prevention is equally if not more important than ILR.
