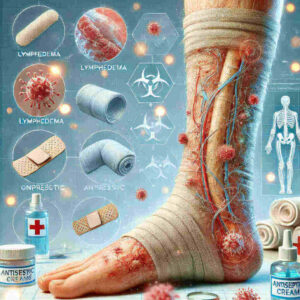
Lymphedema Post-Surgery: Causes, Prevention, and Management
Lymphedema is a condition that many individuals face after surgery, especially in cancer treatments. While it may seem minor, it can significantly impact one’s quality of life. Understanding the causes, prevention strategies, and management options for lymphedema post-surgery is essential to ensuring better patient outcomes. This comprehensive guide will explore the various aspects of lymphedema, focusing on its occurrence after surgeries such as breast cancer treatments and providing expert insights on managing this condition effectively.
Definition of Lymphedema
Lymphedema is a condition characterized by the abnormal accumulation of lymph fluid in the tissues, leading to swelling, usually in the arms or legs. The lymphatic system, which helps maintain fluid balance in the body and fights infections, can become impaired due to surgery, radiation, or injury. This results in lymphedema, which can be either primary (from birth) or secondary. The latter is the most common type, often caused by surgery or cancer treatments.
Importance of Understanding Lymphedema Post-Surgery
Understanding lymphedema post-surgery is vital, especially for patients undergoing cancer treatments, including breast cancer surgeries. After surgery, lymph nodes may be removed or damaged, disrupting the natural flow of lymph fluid and increasing the risk of developing lymphedema. Identifying the causes, preventing its onset, and managing it early on can help reduce complications, prevent chronic conditions, and improve overall patient well-being.
Overview of the Blog Post Structure
This blog post will delve into the causes of lymphedema post-surgery, highlight prevention strategies, and discuss the management options available. We will also touch upon the current trends and treatments that help patients recover and live better post-surgery. Whether you’re a patient, healthcare provider, or caregiver, this guide will equip you with the knowledge to address lymphedema effectively.
Causes of Lymphedema Post-Surgery
Surgical Removal of Lymph Nodes
One of the most common causes of lymphedema after surgery is the removal of lymph nodes, often done during cancer surgeries like breast cancer treatment. Lymph node dissection, which involves the removal of axillary lymph nodes, is typically performed to prevent cancer spread. However, this surgical procedure disrupts the flow of lymph fluid, making it difficult for the body to drain excess fluid properly, resulting in swelling.
Radiation Therapy Effects
Radiation therapy is another significant factor that can cause lymphedema. The radiation used in cancer treatment can damage the lymphatic vessels and lymph nodes, further hindering lymph fluid flow. When the lymphatic system is compromised by radiation, the body’s ability to manage fluid balance is affected, increasing the risk of lymphedema in the treated area. Radiation therapy after breast cancer surgery is a common cause of lymphedema, and patients who undergo both surgery and radiation face an even higher risk.
Infection and Inflammation
Infection and inflammation can also contribute to the development of lymphedema post-surgery. Surgical procedures, particularly those involving the removal of lymph nodes, can increase the risk of infection. Once the lymphatic system is compromised, infections can exacerbate swelling, leading to further damage and a higher risk of lymphedema. Early detection and treatment of infections are crucial to prevent the development of severe swelling and other complications.
Other Contributing Factors
Several other factors can increase the risk of lymphedema, including obesity, genetics, and lifestyle. Individuals who are overweight or have a family history of lymphedema may be more prone to developing this condition after surgery. Furthermore, factors such as sedentary behaviour, poor diet, and lack of regular exercise can contribute to the onset and progression of lymphedema, making it essential to adopt healthy habits for better lymphatic health.
Prevention of Lymphedema
Pre-Surgical Assessments and Planning
Pre-surgical assessments are crucial in identifying patients at a higher risk of developing lymphedema. By evaluating the patient’s overall health, medical history, and risk factors, healthcare providers can develop a tailored plan to minimize the chances of lymphedema post-surgery. For example, specific treatments or surgeries may be adjusted to reduce lymph node removal or prevent excessive radiation exposure, thus lowering the risk of lymphedema.
Techniques to Minimize Lymphatic Damage During Surgery
During surgery, specific techniques can be employed to minimize lymphatic damage. For instance, a less invasive approach may be used, and lymph node transfer or vascularized lymph node transfer can be considered. These procedures aim to restore lymphatic flow and reduce the potential for lymphedema. Surgeons and medical teams are becoming more skilled in these methods, which have shown promising results in preventing post-surgical complications like lymphedema.
Post-Operative Care and Monitoring
Post-operative care plays a crucial role in preventing lymphedema. Early monitoring for signs of swelling and managing the condition proactively can reduce the chances of long-term lymphedema. Patients may be advised to wear compression garments or engage in lymphatic drainage techniques such as manual lymphatic drainage (MLD). Early interventions can significantly reduce the severity and duration of lymphedema if it does occur.
Lifestyle Changes to Reduce Risk
Adopting specific lifestyle changes can also help reduce the risk of lymphedema. Regular physical activity, a healthy weight, and a balanced diet can enhance lymphatic function and overall health. Additionally, avoiding factors that may trigger lymphedema, such as overheating, tight clothing, or injuries, is essential for long-term management.
Management of Lymphedema
Early Detection and Diagnosis
Early detection is key to managing lymphedema effectively. Regular check-ups with a healthcare provider, especially for those who have undergone breast cancer surgery or other lymph node-related treatments, can help detect lymphedema at an early stage. Symptoms of lymphedema often include swelling, tightness, and a feeling of heaviness in the affected area. If these symptoms are recognized early, treatment can begin immediately, reducing the severity of the condition.
Treatment Options
Several effective treatment options are available to manage lymphedema. Compression therapy is one of the most common treatments, and compression garments help reduce swelling and encourage proper lymphatic drainage. Manual lymphatic drainage (MLD) is another therapeutic option, where a trained lymphedema therapist uses specific massage techniques to encourage fluid movement. Surgical treatments such as lymph node transfer or dissection may be considered in more advanced cases.
Role of Physical Therapy and Exercise
Physical therapy and exercise play an essential role in managing lymphedema. A certified lymphedema therapist can work with patients to create customized exercise programs that stimulate lymphatic flow and prevent fluid build-up. Gentle exercises like walking, swimming, or yoga are often recommended to improve overall circulation and lymphatic function. These therapies can be effective in reducing symptoms and improving mobility and function.
Support Resources and Community Programs
Support resources and community programs provide invaluable assistance to individuals living with lymphedema. Support groups offer emotional support, while educational programs help patients and caregivers learn about managing lymphedema. In addition, various online resources and forums provide a platform for individuals to share their experiences, learn from others, and access expert advice.
Conclusion
Lymphedema after surgery, especially following cancer treatments like breast cancer surgery, is a significant concern for many patients. Understanding its causes, prevention strategies, and available treatments can help individuals better manage their health post-surgery. With early detection, proper care, and effective treatment options, individuals can minimize the impact of lymphedema and enjoy an improved quality of life. If you are undergoing surgery or cancer treatment, be sure to discuss your risk of developing lymphedema with your healthcare provider and explore the best strategies for prevention and management.
FAQs
Q: What are the symptoms of lymphedema?
A: The symptoms of lymphedema include swelling in the affected area, a feeling of heaviness or tightness, restricted range of motion, pain, and recurrent infections. Early detection is key for effective lymphedema treatment.
Q: What is the treatment for lymphedema after surgery?
A: The treatment for lymphedema may include compression garments, manual lymphatic drainage, exercise, and skin care. A certified lymphedema therapist can help tailor a treatment plan specific to your needs.
Q: How does breast cancer treatment affect the risk of lymphedema?
A: Breast cancer survivors who undergo surgery or radiation that involves lymph node removal are at a higher risk for lymphedema. Lymphedema can occur when lymph nodes are removed or damaged during treatment.
Q: What types of lymphedema are there?
A: There are two main types of lymphedema: primary lymphedema, which is caused by genetic factors, and secondary lymphedema, which often occurs after surgery or radiation treatment, especially when lymph nodes are removed.
Q: Can lymphedema happen after breast cancer treatment?
A: Yes, lymphedema can occur after breast cancer treatment, especially following surgery to remove lymph nodes or breast surgery. It is important to monitor for signs of lymphedema after treatment for breast cancer.
Q: How can I reduce the risk of lymphedema after surgery?
A: To reduce the risk of lymphedema, patients should follow their doctor’s recommendations, engage in light exercise, maintain a healthy weight, and avoid injury to the affected area. Regular check-ups with a lymphedema therapist can also help.
Q: What surgical options are available for lymphedema?
A: Lymphedema surgery may involve procedures to remove excess tissue or to reconnect lymphatic vessels. The surgical treatment of lymphedema is typically considered for patients with advanced lymphedema when conservative treatments are insufficient.
Q: How can a lymphedema therapist help?
A: A lymphedema therapist can help design a personalized treatment plan, provide manual lymphatic drainage, teach you exercises to improve lymph flow, and give advice on skin care to prevent infections and manage symptoms.
Q: What are the stages of lymphedema?
A: The stages of lymphedema range from mild, where swelling is reversible, to advanced lymphedema, where swelling becomes persistent, and the skin may develop changes. Early intervention is crucial for effective lymphedema treatment.