Live with Lymphedema: Embracing an Active Life with Lymphedema
Living with lymphedema is undoubtedly challenging, but it doesn’t have to limit your ability to lead a fulfilling, active lifestyle. Millions of people worldwide navigate life with this condition, and with the right tools, strategies, and support, you can too. Whether you’re newly diagnosed or have been managing lymphedema for years, this guide is packed with insights to help you embrace your life fully and confidently.
Key Takeaways
- Lymphedema is a chronic condition that requires ongoing care.
- Early recognition of symptoms, such as swelling in an arm or leg, is crucial.
- Effective management involves a combination of self-care, medical treatments, and social support.
- Compression garments and therapies like manual lymphatic drainage (MLD) can significantly help reduce swelling.
- Building a community and maintaining an active lifestyle is essential for overall well-being.
What is Lymphedema and How Does it Affect the Lymphatic System?
Understanding the Lymphatic System and Lymphedema
The lymphatic system is critical in maintaining your body’s fluid balance and immune function. This network of lymph vessels and lymph nodes transports lymph fluid, which contains waste products and immune cells. When this system is disrupted, it can lead to an accumulation of lymph fluid, causing lymphedema.
Lymphedema occurs when damage to the lymphatic system or developmental issues impair this delicate drainage process. It can impact various body parts but commonly affects the arms and legs.
Primary vs. Secondary Lymphedema: What You Need to Know
There are two main types of lymphedema:
- Primary lymphedema is a rare form often caused by genetic factors.
- Secondary lymphedema develops due to external factors like cancer treatment, radiation therapy, or injury.
Understanding these types’ differences helps tailor your lymphedema care and treatment plan.
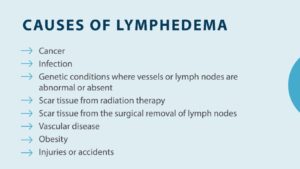
Causes of Lymphedema: Why Does it Happen?
Lymphedema happens for various reasons:
- Primary lymphedema may stem from genetic abnormalities.
- Secondary lymphedema is often linked to breast cancer surgery, damage to the lymphatic system, or infections. Left untreated, lymphedema can lead to complications, including infections and reduced mobility.
What Are the Symptoms of Lymphedema?
Recognizing Early Signs of Lymphedema
Early detection is key. Initial lymphedema symptoms may include:
- Persistent swelling in the affected area, such as an arm or leg.
- A feeling of heaviness or tightness in the limb.
- Difficulty fitting into clothes or shoes due to swelling.
If you notice these signs, consult a healthcare provider for a proper diagnosis.
Common Symptoms: Swelling in the Affected Area
As lymphedema progresses, symptoms can worsen. You might experience:
- Skin changes, such as thickening or hardening.
- Accumulation of lymph fluid, causing significant discomfort.
- Increased risk of signs of infection, such as redness or warmth.
How to Differentiate Between Lymphedema and Other Conditions
Conditions like venous insufficiency or deep vein thrombosis can mimic lymphedema symptoms. A thorough evaluation, including imaging tests and physical exams, can confirm a lymphedema diagnosis.
How to Live with Lymphedema: Strategies for Daily Life
Self-Care Tips for Managing Lymphedema
Living a good life with lymphedema involves consistent self-care practices. These include:
- Keeping the affected area clean and moisturized to prevent skin issues.
- Elevating the limb to support lymphatic drainage.
- Avoid tight clothing or accessories that can restrict fluid flow.
Compression Garments: How They Help Reduce Swelling
Wearing compression garments is a cornerstone of lymphedema management. These garments apply pressure to the limb, helping to:
- Encourage proper lymph fluid movement.
- Help reduce swelling and discomfort.
- Support mobility and function during daily activities.
Exercise and Activity: Staying Active with Lymphedema
Physical activity is not only safe but beneficial for lymphedema patients. Low-impact exercises like swimming, yoga, and walking can:
- Enhance lymphatic fluid circulation.
- Build strength and flexibility without overstraining the affected area.
What Are the Treatment Options for Lymphedema?
Manual Lymphatic Drainage: What to Expect
MLD is a specialized massage technique performed by trained professionals. It gently stimulates the lymphatic system to:
- Improve drainage and reduce fluid buildup.
- Alleviate discomfort and promote relaxation.
Pneumatic Compression: Benefits and Usage
Pneumatic compression devices offer another effective solution. These devices use air pressure to:
- Help move lymphatic fluid out of congested areas.
- Complement other therapies, such as compression bandages and garments.
Working with a Certified Lymphedema Therapist
Collaborating with a lymphedema therapist ensures your treatment plan is tailored to your needs. These specialists:
- Guide proper care techniques.
- Monitor progress and adjust therapies as needed.
How Can Breast Cancer Treatment Lead to Lymphedema?
The Connection Between Breast Cancer and Lymphedema
Breast cancer treatment, especially lymph node removal, increases the risk of lymphedema. Years after cancer treatment, lymphedema may still develop due to lingering effects on the lymphatic system.
Understanding Risk Factors for Developing Lymphedema
Certain factors elevate the risk of lymphedema, including:
- Extensive lymph node removal.
- History of radiation therapy.
- Infections or injuries to the treated area.
Managing Lymphedema After Breast Cancer Treatment
To minimize lymphedema complications post-treatment:
- Regularly wear compression garments.
- Incorporate gentle exercises into your routine.
- Seek support from lymphedema specialists.
What Role Does Social Support Play in Managing Lymphedema?
Finding Community and Resources for People with Lymphedema
Building a network of understanding individuals can make a world of difference. Look for:
- Online forums and local support groups.
- Resources during Lymphedema Awareness Month to stay informed.
How Support Groups Can Help in Lymphedema Management
Joining a support group provides:
- Emotional reassurance from people who truly understand.
- Practical tips for lymphedema management and self-care.
Communicating with Your Healthcare Provider About Lymphedema
Your healthcare provider plays a pivotal role in your care. Regular check-ins allow you to:
- Discuss any new signs of lymphedema or challenges.
- Adjust your treatment plan for optimal results.
FAQ Section
Q: Can untreated lymphedema cause serious problems? A: Yes, left untreated, lymphedema can lead to infections, skin changes, and reduced mobility. Early intervention is essential.
Q: Are there surgical options for lymphedema? A: While there’s no cure for lymphedema, surgical procedures like lymphedema surgery may offer relief in severe cases.
Q: How do I find a certified lymphedema therapist? A: Look for specialists specializing in lymphedema through professional directories or referrals from your healthcare provider.
Q: Is there a specific diet for managing lymphedema? A: A balanced diet with low sodium and rich in anti-inflammatory foods may help reduce swelling and improve overall health.