For breast cancer survivors, navigating life after treatment involves addressing potential side effects, one of which is lymphedema. This article explores the crucial role of physical activity in lymphedema management, offering insights and guidance for those seeking to improve their quality of life. We will discuss the causes, symptoms, and how a tailored exercise program can make a significant difference in reducing lymphedema and improving overall well-being among breast cancer survivors.
Understanding Lymphedema in Breast Cancer Survivors
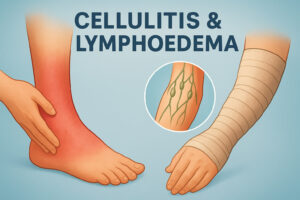
Lymphedema is a chronic condition characterized by swelling, most commonly in the limb, due to a blockage in the lymphatic system. This blockage prevents lymph fluid from draining properly, leading to fluid buildup. Among breast cancer survivors, lymphedema often develops as a result of breast cancer treatment, particularly after surgery or radiation therapy involving the lymph nodes. Understanding this condition is the first step toward effective lymphedema management.
What is Lymphedema?
Lymphedema is not simply ordinary swelling; it’s a specific condition resulting from a compromised lymphatic system. The lymphatic system is a network of vessels and nodes that helps maintain fluid balance and fight infection. When this system is damaged or blocked, lymph fluid accumulates in the tissues, causing lymphedema. This can lead to discomfort, reduced mobility, and increased risk of infection, significantly impacting the quality of life for individuals living with lymphedema.
Causes and Risk Factors
The primary cause of lymphedema in breast cancer survivors is damage to the lymphatic system during breast cancer treatment. Surgical removal of lymph nodes (axillary lymph node dissection) and radiation therapy can disrupt the normal flow of lymph, increasing the risk of lymphedema. Other risk factors include obesity, infection, and trauma to the affected limb. Identifying these factors is crucial for implementing preventive measures and early lymphedema management strategies.
Symptoms and Diagnosis
Recognizing lymphedema symptoms early is essential for prompt intervention. Common signs include swelling in the arm or hand, a feeling of heaviness or tightness, aching or discomfort, and skin changes such as thickening or hardening. Diagnosis typically involves a physical examination and measurement of the affected limb compared to the unaffected limb. In some cases, imaging tests like lymphoscintigraphy may be used to assess the function of the lymphatic system. Early detection is key to effective lymphedema treatment and minimizing long-term complications.
The Importance of Physical Activity
Physical activity plays a vital role in lymphedema management for breast cancer survivors. Contrary to previous beliefs, appropriate exercise can help improve lymph flow and reduce lymphedema. A carefully designed exercise program, including both aerobic exercise and resistance exercise, can enhance lymphatic drainage, improve muscle strength, and boost overall well-being, significantly impacting the quality of life of survivors with lymphedema.
How Physical Activity Affects Lymphedema
Physical activity positively influences lymphedema by stimulating the lymphatic system. Muscle contractions during exercise help to pump lymph fluid through the vessels, reducing swelling and preventing fluid buildup. Aerobic exercise, such as walking or swimming, increases overall circulation, while resistance exercise strengthens muscles and further supports lymphatic drainage. This combined approach can effectively reduce lymphedema and improve limb function for people with lymphedema.
Research on Exercise and Lymphedema Management
Extensive cancer research supports the benefits of physical activity in lymphedema management. A systematic review of randomized controlled trial studies has shown that exercise intervention, including aerobic and resistance exercise, does not worsen lymphedema and can actually reduce lymphedema, lymphedema symptoms, and improve limb volume. These findings have led to a paradigm shift in lymphedema care, with exercise programs now recognized as an integral part of comprehensive lymphedema treatment. Always consult your doctor before beginning any exercise routine.
The Power of Exercise for Quality of Life
Beyond the physical benefits, the power of exercise extends to improving the overall quality of life for breast cancer survivors with lymphedema. Regular physical activity can reduce fatigue, improve mood, enhance self-esteem, and promote better sleep. By taking an active role in their lymphedema management, individuals living with lymphedema can regain a sense of control and empowerment, leading to a more fulfilling and active lifestyle.
Types of Exercise Beneficial for Lymphedema
Incorporating the right types of exercise is paramount for effective lymphedema management in breast cancer survivors. Different forms of physical activity offer unique benefits, from enhancing lymph flow to improving muscle strength and flexibility. A well-rounded exercise program typically includes aerobic exercise, resistance exercise, and flexibility exercises, all tailored to the individual’s needs and lymphedema status. Consulting a certified lymphedema therapist or healthcare professional is crucial before starting any exercise program.
Aerobic Exercises
Aerobic exercise plays a key role in managing lymphedema. Activities like walking, swimming, cycling, and dancing elevate the heart rate and increase overall circulation, promoting lymphatic drainage. The rhythmic muscle contractions during aerobic exercise help to pump lymph fluid through the lymphatic system, reducing swelling and preventing fluid buildup. Aim for at least 30 minutes of moderate-intensity aerobic exercise most days of the week, gradually increasing duration and intensity as tolerated. A regular exercise routine is a key element in improving the quality of life.
Strength Training
Resistance training, also known as strength training, is another essential component of an exercise program for breast cancer survivors with lymphedema. Strengthening exercises, such as lifting weights or using resistance bands, improve muscle strength and tone, which further supports lymphatic drainage. Stronger muscles help to compress lymph vessels, facilitating the movement of lymph fluid and reducing lymphedema. It is important to work with a certified lymphedema therapist or qualified healthcare professional to ensure proper form and technique. Strength training should always be performed under appropriate guidance for the affected limb.
Flexibility and Stretching Exercises
Flexibility and stretching exercises are crucial for maintaining range of motion and preventing stiffness in the affected limb. Stretching helps to improve lymph flow by reducing muscle tension and promoting tissue flexibility. Gentle stretching exercises, such as yoga or tai chi, can be particularly beneficial for individuals living with lymphedema. Incorporating regular stretching into your exercise session can improve overall comfort, reduce pain, and enhance the quality of life by addressing lymphedema symptoms. This holistic approach is a cornerstone of effective lymphedema care and should be part of every exercise program.
Exercise Recommendations for Breast Cancer Survivors
For breast cancer survivors, embarking on a physical activity journey post-treatment requires thoughtful consideration and personalized guidance. The right exercise routine can significantly improve lymphedema management and overall well-being. However, it’s essential to approach exercise intervention safely and effectively. Tailoring your activities to your individual needs, consulting with healthcare professionals, and listening to your body are crucial steps to ensure you reduce lymphedema while enhancing your quality of life. Proper planning and execution are key to a successful exercise routine for patients with lymphedema.
Guidelines for Safe Exercise
Safety should always be a top priority when engaging in physical activity for lymphedema management. It’s recommended that breast cancer survivors consult with a certified lymphedema therapist or healthcare provider before starting any exercise program. They can assess your individual needs, lymphedema status, and overall health to develop a safe and effective plan. Start slowly and gradually increase the intensity and duration of your workouts. Wearing a properly fitted compression garment during exercise help to support lymph flow and reduce swelling.
Frequency and Duration of Physical Activity
Consistency is key when it comes to the frequency and duration of physical activity for lymphedema management. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week. Incorporate resistance exercise at least two days per week, focusing on major muscle groups. Each exercise session should include a warm-up, cool-down, and stretching exercises. Listen to your body and adjust the frequency and duration as needed, prioritizing comfort and safety to effectively reduce lymphedema.
Listening to Your Body: Signs to Stop or Modify
Paying close attention to your body’s signals is crucial during physical activity. If you experience any new or worsening lymphedema symptoms, such as increased swelling, pain, heaviness, or tightness in the affected limb, stop exercising immediately. Consult with your certified lymphedema therapist or healthcare provider to determine the cause and adjust your exercise routine accordingly. It may be necessary to modify the intensity, duration, or type of exercise to ensure your safety and comfort. Remember, exercise can help, but should never exacerbate lymphedema.
Enhancing Lymphedema Management with Compression
The Role of Compression Garments
Compression garments play a critical role in lymphedema management for breast cancer survivors. These specialized garments provide external pressure to the affected limb, aiding in lymph fluid drainage and reducing swelling. By gently squeezing the tissues, compression garments support the lymphatic system, preventing fluid from accumulating and improving overall limb volume. Regular use of compression is often recommended as part of a comprehensive lymphedema treatment plan, especially during physical activity.
When to Use Compression During Exercise
Using compression during exercise sessions is highly beneficial for breast cancer survivors with lymphedema. Wearing a compression garment during aerobic exercise or resistance exercise helps to support lymph flow and minimize swelling. The external pressure provided by the compression enhances the pumping action of muscles, facilitating lymph fluid drainage. It is generally recommended to wear a well-fitted compression garment throughout your exercise routine to maximize its benefits and reduce lymphedema, thus increasing quality of life.
Choosing the Right Compression Garment
Selecting the right compression garment is essential for effective lymphedema management. It is important to consult with a certified lymphedema therapist to determine the appropriate type, size, and level of compression for your individual needs. Compression garments come in various styles, including sleeves, gloves, stockings, and custom-made options. A proper fit is crucial to ensure comfort and effectiveness. Your certified lymphedema therapist can guide you in choosing a compression garment that provides adequate support without restricting movement, further improving quality of life.
Practical Tips for Integrating Exercise into Daily Life
Creating a Sustainable Exercise Routine
Creating a sustainable exercise routine is essential for long-term lymphedema management in breast cancer survivors. Start by setting realistic goals and gradually increasing the intensity and duration of your workouts. Find activities you enjoy to make physical activity a more enjoyable part of your daily life. Incorporate both aerobic exercise and resistance exercise, as well as flexibility exercises, for a well-rounded approach. Consistency is key, so aim for regular exercise sessions to maintain the benefits and improve your quality of life.
Finding Support and Resources
Finding support and resources can significantly enhance your lymphedema management journey. Connect with other breast cancer survivors through support groups or online communities to share experiences and gain encouragement. Work closely with a certified lymphedema therapist to develop a personalized exercise program and receive ongoing guidance. Utilize resources such as cancer research centers, lymphedema organizations, and healthcare professionals to stay informed and access the best possible care in order to reduce lymphedema and improve quality of life.
Utilizing Technology and Apps for Motivation
Utilizing technology and apps can be a great way to stay motivated and track your progress with physical activity. Fitness trackers and smartphone apps can help you monitor your activity levels, set goals, and receive reminders to exercise. Many apps also offer guided workouts, personalized training plans, and social features that allow you to connect with other breast cancer survivors. By leveraging these technological tools, you can make exercise help in lymphedema management more engaging and sustainable, further helping improve quality of life among breast cancer survivors.
Conclusion and Key Takeaways
Recap of the Benefits of Physical Activity
In summary, physical activity offers significant advantages for breast cancer survivors dealing with lymphedema. A well-structured exercise program, incorporating both aerobic exercise and resistance exercise, can stimulate the lymphatic system, promoting lymph drainage and reducing swelling. Exercise helps improve muscle strength and flexibility while also enhancing the quality of life by reducing fatigue and boosting overall well-being. The combined effect of exercise makes it a cornerstone of effective lymphedema management and should be encouraged among breast cancer survivors.
Final Advice for Breast Cancer Survivors
For breast cancer survivors navigating lymphedema management, remember that consistency and self-care are paramount. Always consult with a certified lymphedema therapist before starting any exercise program and listen to your body’s signals. Incorporate compression, stay hydrated, and prioritize activities you enjoy to make physical activity a sustainable part of your routine. By taking an active role in your care and embracing a holistic approach, you can effectively reduce lymphedema and improve your quality of life while living with breast cancer.
Frequently Asked Questions (FAQs)
1. Can exercise really help reduce lymphedema?
Yes, exercise can help reduce lymphedema. While it was once thought that physical activity could worsen the condition, current research shows that a carefully designed exercise program, including both aerobic and resistance exercise, can stimulate the lymphatic system, promoting lymph drainage and reducing swelling in the affected limb. It’s crucial to work with a certified lymphedema therapist to ensure the exercise routine is safe and effective for your individual needs to properly engage in lymphedema management.
2. What types of exercises should I avoid?
While exercise helps in lymphedema management, certain activities may exacerbate lymphedema symptoms. Avoid strenuous activities that cause excessive strain or impact on the affected limb, as well as exercises that involve prolonged repetitive motions or heavy lifting without proper compression. It’s essential to listen to your body and stop any activity that causes increased swelling, pain, or discomfort. A certified lymphedema therapist can provide personalized guidance on types of exercise to avoid for breast cancer survivors.
3. How often should I exercise for lymphedema management?
For effective lymphedema management, aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week. Incorporate resistance exercise at least two days per week, focusing on major muscle groups. Each exercise session should include a warm-up, cool-down, and stretching exercises. Consistency is key, but listen to your body and adjust the frequency and duration as needed to effectively reduce lymphedema without overexerting yourself. Remember that exercise helps, but only when performed safely.
4. Are there specific exercises recommended for swelling in limbs?
Yes, there are specific exercises recommended for swelling in the limb due to lymphedema. These typically include gentle aerobic exercise like walking, swimming, or cycling, as well as resistance exercise using light weights or resistance bands. Range-of-motion exercises and stretching can also help improve lymph flow and reduce stiffness. Consult with a certified lymphedema therapist to develop a personalized exercise program that targets the specific areas of swelling and addresses your individual needs so you may improve your quality of life.
5. How do I choose the right compression garment for exercise?
Choosing the right compression garment for exercise is crucial for effective lymphedema management. Consult with a certified lymphedema therapist to determine the appropriate type, size, and level of compression for your individual needs. The compression garment should provide adequate support without restricting movement or causing discomfort. Consider features such as breathability, moisture-wicking properties, and ease of application. Your certified lymphedema therapist can guide you in selecting a compression garment that enhances your exercise routine and minimizes swelling, ensuring exercise helps.