Introduction To Genital Lymphedema:
Genital lymphedema is a rare and often distressing medical condition that causes swelling of the external genital organs due to impaired lymphatic drainage. Although uncommon, it can lead to physical discomfort, difficulty with mobility, sexual dysfunction, and psychological stress.
This article provides a detailed overview of genital lymphedema, including its causes, risk factors, symptoms, diagnostic methods, and current treatment options. The content is intended for educational purposes only and is not a substitute for medical advice. Always consult a qualified healthcare professional for a personalised diagnosis and treatment.
What Is Genital Lymphedema?
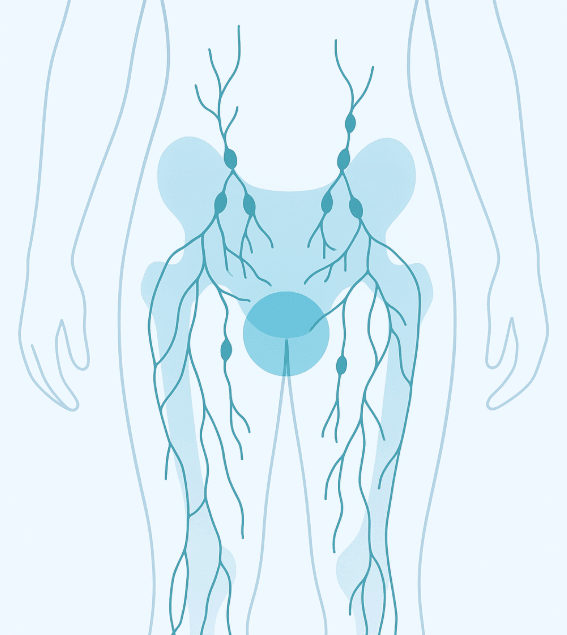
Lymphedema is the abnormal buildup of protein-rich lymphatic fluid in soft tissues due to impaired lymphatic circulation. When this occurs in the genital area—affecting the scrotum, penis, vulva, or labia—it is classified as genital lymphedema.
The condition can present at birth (primary lymphedema) or develop later in life (secondary lymphedema). While genital lymphedema is rare compared to limb lymphedema, it can be especially challenging to manage due to the sensitivity and function of the affected region.
Causes of Genital Lymphedema
1. Primary Lymphedema
Primary genital lymphedema results from congenital abnormalities in lymphatic vessel development. It may manifest in childhood, adolescence, or early adulthood. Genetic syndromes such as Milroy disease and Meige disease are sometimes associated with primary lymphedema.
2. Secondary Lymphedema
Secondary genital lymphedema develops due to damage or obstruction of lymphatic vessels. Common causes include:
- Cancer treatments: Surgery or radiation for pelvic cancers (prostate, bladder, cervical, uterine, vulvar) can disrupt lymphatic drainage.
- Infections: Recurrent cellulitis or parasitic infections such as lymphatic filariasis (endemic in parts of Asia and Africa) are major global contributors.
- Trauma or surgery: Pelvic or groin injuries may damage lymphatic vessels.
- Obesity: Excess body weight may increase lymphatic load and worsen fluid buildup.
Risk Factors
While genital lymphedema can affect anyone, certain factors increase the likelihood:
- Previous pelvic surgery or lymph node dissection
- Radiation therapy in the pelvic or groin region
- Chronic skin infections
- Obesity and metabolic syndrome
- Genetic predisposition to lymphatic dysfunction
Symptoms of Genital Lymphedema
The condition often develops gradually, but in some cases swelling appears rapidly. Common symptoms include:
- Persistent swelling of the scrotum, penis, vulva, or labia
- Heaviness or discomfort in the affected area
- Restricted mobility and difficulty walking or sitting
- Skin thickening (fibrosis) or changes in texture
- Recurrent infections (cellulitis, fungal infections)
- Emotional distress, embarrassment, or reduced quality of life
Diagnosis of Genital Lymphedema
A diagnosis usually involves a combination of clinical evaluation and imaging:
- Physical examination to assess swelling, skin changes, and history of previous medical conditions.
- Imaging studies such as MRI, ultrasound, or lymphoscintigraphy to evaluate lymphatic vessel function.
- Exclusion of other conditions like hernias, tumors, or fluid retention due to systemic disease.
Early diagnosis is essential, as timely intervention can prevent progression and complications.
Treatment Options for Genital Lymphedema
Currently, there is no definitive cure for lymphedema. However, a variety of treatment approaches can manage symptoms, reduce swelling, and improve quality of life.
Conservative (Non-Surgical) Management
- Manual Lymphatic Drainage (MLD): A specialized massage technique performed by trained therapists to promote lymphatic flow.
- Compression Therapy: Use of custom-made compression garments or bandaging to reduce swelling. (Note: Compression in the genital region may be difficult; specialized garments are available.)
- Exercise and Physiotherapy: Gentle, guided exercises help improve circulation and lymphatic flow.
- Skin Care: Daily hygiene and moisturization reduce infection risk.
- Medications: Antibiotics may be prescribed for infections; however, no drug can directly cure lymphedema.
Surgical Management
When conservative measures fail, surgery may be considered:
- Excisional surgery: Removal of excess fibrotic tissue.
- Lymphatic reconstruction: Advanced microsurgical procedures such as lymphovenous bypass or vascularized lymph node transfer.
- Scrotal reduction surgery: For cases of massive scrotal lymphedema impairing mobility.
These surgeries are highly specialized and usually performed at tertiary care centers with experience in lymphatic disorders.
Living With Genital Lymphedema
Managing genital lymphedema requires ongoing care:
- Maintaining healthy weight
- Preventing infections with good hygiene
- Wearing supportive undergarments or compression devices if recommended
- Seeking psychological support or counseling to cope with emotional challenges
- Regular follow-ups with a lymphedema specialist
Psychological and Social Impact
Beyond physical discomfort, genital lymphedema can cause significant psychological distress:
- Embarrassment and stigma due to visible swelling
- Anxiety or depression related to body image
- Impact on intimate relationships and sexual health
Counselling, patient support groups, and open discussions with healthcare providers can help address these challenges.
Prevention and Early Detection
While not all cases can be prevented, risk reduction strategies include:
- Careful monitoring after cancer surgery or radiation
- Prompt treatment of infections
- Weight management and a healthy lifestyle
- Patient education about early symptoms of swelling
When to See a Doctor
Seek medical attention if you experience:
- Unexplained swelling in the genital area
- Recurrent skin infections or discomfort
- Rapid enlargement or sudden worsening of symptoms
- Difficulty with mobility or hygiene due to swelling
Conclusion
Genital lymphedema is a rare but serious condition with significant physical, emotional, and social consequences. While there is currently no cure, a combination of conservative therapies and surgical interventions can greatly improve symptoms and quality of life. Early recognition, professional diagnosis, and multidisciplinary care are essential for optimal management.
Disclaimer
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek guidance from a licensed healthcare provider if you suspect you have genital lymphedema or any other medical condition.
References:
- Cleveland Clinic. Genital Lymphedema – ClevelandClinic.org
- Tampa General Hospital. Genital Lymphedema – TGH.org
- International Society of Lymphology. Consensus Document for the Diagnosis and Treatment of Peripheral Lymphedema, 2020.
- Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008.
- Damstra RJ, et al. Surgical management of primary genital lymphedema. J Plast Reconstr Aesthet Surg. 2009.