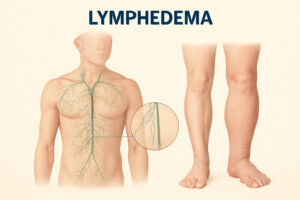
Lymphedema is a condition that results in swelling, typically in the arms or legs, due to the buildup of lymphatic fluid in the tissues. While it is often associated with factors like surgery, radiation, or infections, there is also a genetic component to the development of lymphedema. In this article, we will explore the genetic basis of lymphedema, focusing on how inherited factors contribute to the condition, how it is passed through families, and what scientific research reveals about this connection.
What is Lymphedema?
Lymphedema occurs when the lymphatic system, which helps the body eliminate waste and toxins, becomes impaired. This system consists of lymph nodes and vessels that carry lymph fluid throughout the body. When these lymphatic structures are damaged or malformed, lymph fluid accumulates, resulting in swelling.
Primary vs. Secondary Lymphedema
Lymphedema is generally classified into two types:
- Primary Lymphedema: This form is caused by congenital malformations or genetic mutations that affect the development of the lymphatic system.
- Secondary Lymphedema: This form results from external factors such as surgery, trauma, radiation, or infections that damage the lymphatic system.
This article will specifically focus on primary lymphedema, which has a clear genetic basis.
The Role of Genetics in Lymphedema
Primary lymphedema is typically inherited and passed down from generation to generation through genetic mutations. These mutations affect the development and functioning of the lymphatic system, leading to abnormal lymphatic drainage and fluid accumulation.
Genetic mutations that cause primary lymphedema often affect the proteins or enzymes involved in developing and maintaining the lymphatic vessels and nodes. Depending on the specific gene, these mutations can be present from birth or later in life.
Inherited Patterns of Lymphedema
Lymphedema caused by genetic mutations can follow different patterns of inheritance, which can impact how the condition is passed down through families.
- Autosomal Dominant Inheritance: In some cases, lymphedema is inherited in an autosomal dominant pattern, meaning that only one copy of the mutated gene is necessary for the condition to develop. If one parent carries the mutation, there is a 50% chance of passing it on to each child.
- Autosomal Recessive Inheritance: Other forms of primary lymphedema follow an autosomal recessive inheritance pattern, meaning that both gene copies must be mutated for the condition to manifest. In these cases, both parents must be carriers of the mutation for their child to inherit the condition.
- X-linked Inheritance: Some rare forms of lymphedema follow an X-linked inheritance pattern, which is typically passed down through the maternal side and affects males more severely than females.
Understanding these inheritance patterns is crucial for genetic counseling and predicting the likelihood of developing lymphedema in individuals with a family history of the condition.
Key Genes Involved in Lymphedema
Several genes have been identified that are linked to the development of primary lymphedema. These genes are responsible for the formation and maintenance of the lymphatic system. Mutations in these genes can lead to malformations or dysfunctions in the lymphatic vessels, resulting in lymphedema.
1. FLT4 (VEGFR-3) Gene
The FLT4 gene provides instructions for making a vascular endothelial growth factor receptor 3 (VEGFR-3) protein. This protein is essential for developing the lymphatic system, as it helps lymphatic vessels grow and maintain their function. Mutations in the FLT4 gene can lead to abnormal lymphatic vessel formation, causing primary lymphedema.
How FLT4 Mutations Lead to Lymphedema
Mutations in FLT4 can impair the signaling required for proper lymphatic vessel formation. As a result, the lymphatic vessels may be too few, malformed, or not fully functional, leading to fluid accumulation and swelling, which are hallmark symptoms of lymphedema.
2. PIEZO1 Gene
The PIEZO1 gene encodes a protein that functions as a mechanosensitive ion channel, sensing mechanical changes in tissues. PIEZO1 mutations are associated with primary lymphedema, known as hereditary lymphedema type 2.
Mechanisms of PIEZO1 Mutations
PIEZO1 mutations affect the ability of lymphatic vessels to handle the pressure exerted by the fluid they transport. This leads to dysfunction in the lymphatic system, impairing the ability to clear excess fluid from the tissues and causing swelling in the affected areas.
3. CCBE1 Gene
The CCBE1 gene is involved in developing the lymphatic system and organizing lymphatic vessels. Mutations in this gene have been linked to Congenital Lymphedema, a type of lymphedema present at birth.
Role of CCBE1 in Lymphatic Development
CCBE1 mutations disrupt the formation of lymphatic vessels during fetal development, leading to malformed or insufficient lymphatic drainage. As a result, lymph fluid accumulates in the affected tissues, causing swelling and other related symptoms.
4. VE-cadherin (CDH5) Gene
The VE-cadherin gene, also known as CDH5, codes for a protein that maintains the integrity of blood vessels, including those in the lymphatic system. Mutations in this gene have been associated with vascular-related forms of lymphedema.
Impact of CDH5 Mutations
When CDH5 is mutated, it impairs the function of endothelial cells that line the lymphatic vessels. This can lead to poor vessel formation and insufficient fluid drainage, contributing to lymphedema.
How Genetic Testing Can Help Diagnose Lymphedema
Genetic testing has become a valuable tool for diagnosing primary lymphedema. By identifying mutations in the key genes mentioned above, healthcare providers can confirm a diagnosis of genetic lymphedema and determine the most appropriate course of treatment.
Benefits of Genetic Testing
- Accurate Diagnosis: Genetic testing can help confirm the underlying cause of lymphedema, especially in cases with a familial history or without any known external causes.
- Personalized Treatment: Knowing the genetic mutation allows more targeted treatment and management strategies.
- Family Planning: Genetic testing can help individuals with a family history of lymphedema understand the risk of passing the condition to their children.
Genetic Counselling for Lymphedema
Genetic counseling is an essential service for individuals with a family history of lymphedema. A genetic counselor can help individuals understand the genetic basis of their condition, assess their risk of passing it on to future generations, and provide support for making informed decisions about family planning.
How Genetic Counselling Works
During a genetic counseling session, a trained counselor will review the family history, discuss potential genetic testing options, and explain the implications of the results. They may also guide lifestyle modifications and management options for those diagnosed with genetic lymphedema.
Current Research on Genetic Lymphedema
Research into the genetic causes of lymphedema is ongoing, with discoveries and insights being made regularly. Scientists are working to understand better the specific genetic mutations that cause primary lymphedema and to develop more effective treatments. Advances in gene therapy and targeted therapies offer hope for individuals with genetic forms of lymphedema, potentially leading to improved management and even cures in the future.
Conclusion
Lymphedema is a complex condition with environmental and genetic components. Understanding its genetic basis is essential for diagnosing it, developing effective treatments, and providing support for individuals and families affected by it. As research continues to uncover the underlying genetic causes of lymphedema, it is hoped that more precise therapies and management strategies will emerge, offering improved outcomes for those living with this condition.
FAQs
Q1: Is lymphedema always genetic?
No, lymphedema can be caused by genetic factors (primary lymphedema) and external factors such as surgery, radiation, or injury (secondary lymphedema).
Q2: Can genetic testing help determine if I have lymphedema?
Genetic testing can help identify mutations in specific genes linked to primary lymphedema, providing an accurate diagnosis.
Q3: Can lymphedema be prevented with genetic testing?
While genetic testing can help identify those at risk, lymphedema caused by genetic mutations cannot be prevented. However, early diagnosis allows for better management.
Q4: Are there treatments available for genetic lymphedema?
There is no cure for genetic lymphedema, but treatments like compression therapy, manual lymphatic drainage, and exercise can help manage symptoms.
Q5: How can genetic counselling help individuals with lymphedema?
Genetic counselling helps individuals understand the inheritance patterns of lymphedema, assess risks for future generations, and make informed decisions about family planning and management strategies.