Lymphedema is one of those conditions that can slip under the radar, even for seasoned healthcare professionals. It’s not as headline-grabbing as heart disease or diabetes, but for patients dealing with swollen limbs and chronic discomfort, it’s a life-altering reality. Proper care can make all the difference, yet many providers lack the specialized knowledge to manage it effectively. Why is education so critical in lymphedema care, and how does it shape patient outcomes? This article examines the crucial role of training for healthcare professionals, encompassing everything from understanding the condition to delivering compassionate and effective treatment.
What Is Lymphedema?
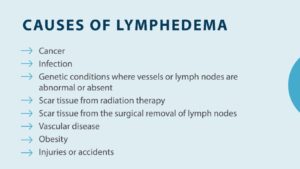
Lymphedema occurs when the lymphatic system, which drains excess fluid from tissues, gets blocked or damaged. The result is swelling, often in the arms or legs, that can feel heavy, tight, or painful. It’s commonly linked to cancer treatments like lymph node removal or radiation, but it can also stem from infections, injuries, or genetic disorders. For patients, it’s not just a physical issue—lymphedema can erode confidence, limit mobility, and increase the risk of infection.
Healthcare professionals encounter lymphedema in various settings, from oncology clinics to primary care offices. Yet, without proper training, they might misdiagnose it as regular swelling or overlook its emotional toll. Education bridges this gap, equipping providers with the tools to recognize and treat the condition early before it spirals into something more complex to manage.
Why Education Matters in Lymphedema Care
Lymphedema isn’t a condition you can manage on your own. It’s complex, chronic, and requires a nuanced approach. Without specialized training, healthcare professionals might rely on outdated methods or miss critical signs, leaving patients frustrated and undertreated. Education ensures providers understand the condition’s intricacies, from its causes to its long-term impact, so they can offer care that’s both effective and empathetic.
Think about it: a patient with a swollen arm after breast cancer surgery needs more than a generic prescription. They need a provider who knows how to assess the swelling, recommend therapies, and address their fears about living with a visible condition. Training makes this possible, turning good intentions into tangible results. It’s the difference between a patient feeling heard and one feeling dismissed.
The Knowledge Gap in Healthcare
Here’s the reality: lymphedema isn’t a primary focus in most medical or nursing school curricula. A doctor might get a brief lecture on the lymphatic system, but the nitty-gritty of lymphedema management—staging, therapy techniques, or patient counseling—often comes later, if at all. Physical therapists, nurses, and even oncologists can graduate without ever learning how to fit a compression garment or perform manual lymph drainage. This gap leaves providers unprepared when patients arrive with swollen limbs and urgent questions.
One nurse I heard about admitted she felt lost when her patient asked about lymphedema after surgery. She’d never been taught how to guide them beyond basic wound care. Specialized education fills this void, giving professionals the confidence to handle cases they’d otherwise fumble. It’s not about memorizing facts—it’s about knowing how to act when a patient’s quality of life is on the line.
Key Areas of Lymphedema Education
Effective lymphedema care necessitates a comprehensive examination of several key areas. Training programs, whether through certifications or continuing education, cover the essentials that healthcare professionals need to master. These aren’t just academic exercises—they’re practical skills that directly improve patient care.
Understanding the Lymphatic System
It all starts with the lymphatic system. Providers need to grasp how it works, why it fails, and how blockages lead to swelling. This isn’t just biology 101—it’s about connecting the dots between a patient’s medical history and their symptoms. For example, knowing that radiation can scar lymph vessels helps a doctor explain why swelling started months after treatment. Education demystifies the system, making it easier to diagnose and treat.
Diagnosis and Staging
Diagnosing lymphedema isn’t always straightforward. It can look like other conditions, like venous edema or heart failure, which is why training emphasizes differential diagnosis. Tests like lymphoscintigraphy or bioimpedance spectroscopy are tools providers learn to use or interpret. Staging—classifying lymphedema from mild (Stage 1) to severe (Stage 3)—is another critical skill, as it guides treatment plans. A well-educated provider can identify Stage 1 swelling early, thereby preventing its progression to more advanced stages.
Complete Decongestive Therapy (CDT)
CDT is the gold standard for lymphedema treatment, combining manual lymph drainage, compression, exercise, and skincare. Training in CDT is hands-on, teaching providers how to perform gentle massages that redirect lymph fluid or fit compression garments that don’t pinch or irritate. It’s not just technique—education covers how to teach patients to do self-care at home. One therapist shared how her CDT training helped a patient reduce leg swelling enough to wear shoes comfortably again—a small victory with a significant impact.
Patient Education and Counseling
Lymphedema is a lifelong condition, so patients need to understand their role in managing it. Educated providers know how to explain the condition without overwhelming someone. They can explain why compression is necessary and how to recognize an infection. Counseling skills are just as crucial—lymphedema can significantly impact self-esteem, and a trained professional knows how to listen, validate, and guide individuals effectively. It’s about building trust, not just prescribing a sleeve.
The Impact of Education on Patient Outcomes
When healthcare professionals are well-trained, patients win. Education leads to earlier diagnoses, better treatment plans, and fewer complications. It’s not just about reducing swelling—it’s about helping people live fuller lives. Let’s look at how this plays out.
Early Detection and Intervention
Trained providers catch lymphedema before it becomes severe. They know to check for subtle signs, such as a slightly puffy hand, and act quickly with therapies like CDT. Early intervention can prevent swelling from progressing to Stage 1, thereby sparing patients the pain and mobility issues associated with later stages of the condition. One study found that patients treated by lymphedema-certified therapists had a 30 percent lower risk of infections, a common complication. That’s the power of education in action.
Reduced Complications
Lymphedema patients face risks, including cellulitis, a skin infection that can lead to hospitalization. Educated providers teach patients how to care for their skin and recognize warning signs, such as redness or warmth, to help them maintain healthy skin. They also know how to adjust treatments to prevent flare-ups. For example, a trained nurse might notice a compression garment is too tight and fix it before it causes harm. These minor adjustments add up, keeping patients healthier.
Improved Quality of Life
Lymphedema isn’t just physical, it affects mental health, relationships, and daily routines. Providers with proper training can address the whole picture. They might suggest aquatic therapy for a patient who enjoys swimming or connect them to a support group to help ease isolation. One patient I read about said her therapist’s encouragement helped her wear shorts again, something she hadn’t done in years. Education empowers providers to make these life-changing moments possible.
Challenges in Lymphedema Education
Despite its importance, lymphedema education faces hurdles. Access to training is a big one—not every provider has the time, money, or opportunity to get certified. Programs can cost thousands of dollars and require weeks of study, which is tough for busy professionals. Rural areas often lack training centers, forcing providers to travel or rely on online courses that might not include hands-on practice.
Another challenge is awareness. Some healthcare professionals don’t even realize they need lymphedema training until they’re faced with a patient they can’t help. Medical schools and nursing programs could do more to highlight the condition, but more common diseases often overshadow it. Overcoming these barriers requires advocacy, funding, and a shift in how we prioritize the management of chronic conditions.
Cost and Time Barriers
Let’s be real—training isn’t cheap. A lymphedema certification course may cost $3,000 or more, excluding travel and lost work time. For a physical therapist juggling a full caseload, that’s a tough sell. Employers could help by subsidizing costs or offering paid leave, but not all do. Online courses are more affordable but often lack the practical component, like learning to bandage a swollen leg. Balancing cost and quality is a puzzle that needs to be solved.
Keeping Skills Current
Lymphedema care continues to evolve, with new research on therapies such as pneumatic compression and surgical options. Trained providers must stay up-to-date, which requires ongoing education. Conferences, webinars, and journals are helpful, but they need time. One doctor I know sets aside an hour a week to read up on lymphedema studies—it’s a small habit that keeps her sharp. Making continuing education accessible and engaging is key to long-term success.
How to Access Lymphedema Training
So, where do healthcare professionals go to get educated? Several paths are available, ranging from formal certifications to shorter workshops. Organizations such as the Lymphology Association of North America and the Academy of Lymphatic Studies offer comprehensive programs that often combine online theory with in-person practice. These cover everything from anatomy to advanced CDT techniques.
For those not yet ready for full certification, continuing education credits obtained through webinars or conferences are a good starting point. Some hospitals offer in-house training, particularly in oncology or rehabilitation departments. The catch? Providers need to be proactive. Seeking out mentors or joining professional networks can point you to the right resources. It’s about taking ownership of your learning.
The Role of Interdisciplinary Training
Lymphedema care isn’t just for one type of provider. Doctors, nurses, physical therapists, and even mental health counselors all play a role. Interdisciplinary training brings these groups together, fostering teamwork. For example, a workshop might teach a nurse how to identify early lymphedema and a therapist how to perform CDT, ensuring everyone is on the same page. This approach leads to better-coordinated care, which patients notice.
The Patient’s Perspective
Patients feel the direct impact of educated providers. A well-trained professional doesn’t just treat swelling—they listen, explain, and adapt their approach. They know how to calm a patient’s fears about a new diagnosis or adjust a treatment plan when life gets in the way. One patient shared how her therapist’s training made all the difference—she went from feeling hopeless to managing her lymphedema with confidence. That’s what education does: it turns clinical care into human connection.
Empowering Patients Through Education
Trained providers don’t just treat—they teach. They show patients how to perform self-massage, select the right compression gear, and exercise safely. This empowerment is huge. A patient who understands their condition is more likely to adhere to treatment, thereby reducing the likelihood of complications. It’s a ripple effect: educated providers create educated patients, and everyone benefits.
The Future of Lymphedema Education
The field of lymphedema care is growing, and education is keeping pace with it. Online platforms are making training more accessible, and research is refining best practices to enhance the learning experience. Advocacy groups are pushing for lymphedema to be a more prominent part of medical education, which could mean that more providers enter the workforce ready to help. The goal? A world where no patient hears, “I’m not sure what to do about your swelling.”
Conclusion
Education is the backbone of quality lymphedema care. It equips healthcare professionals to diagnose early, treat effectively, and support patients holistically. From mastering CDT to counseling with empathy, training turns good providers into great ones. For patients, this means less pain, fewer complications, and a better quality of life. Investing in education isn’t just about building skills; it’s about building hope. Got questions? Here are some answers to dive deeper.
FAQs
Q1: Why do healthcare professionals need special training for lymphedema?
Lymphedema is complex and often misdiagnosed. Training teaches providers to recognize, treat, and manage it effectively, improving patient outcomes.
Q2: What’s involved in lymphedema certification?
Certification includes learning about the lymphatic system, diagnosis, Complete Decongestive Therapy, and patient education, often with hands-on practice.
Q3: Can nurses and therapists both get lymphedema training?
Yes, training is open to doctors, nurses, therapists, and other healthcare professionals. Interdisciplinary programs ensure everyone can contribute to care.
Q4: How does provider education help lymphedema patients?
Educated providers can detect lymphedema early, minimize complications, and equip patients with self-care skills, thereby enhancing their quality of life.
Q5: Where can professionals find lymphedema training?
Organizations like the Academy of Lymphatic Studies offer certifications, while webinars and hospital workshops provide shorter, more accessible options for learning.